AI prediction pediatric cancer is revolutionizing the way we approach the detection and management of childhood cancers, particularly in the realm of brain tumors such as pediatric gliomas. A recent study from Mass General Brigham highlights the efficacy of an innovative AI tool designed to analyze multiple MRI scans over time, yielding more accurate predictions of cancer recurrence than traditional methods. This significant advancement in artificial intelligence in medicine showcases the potential for improved treatment protocols that not only enhance outcomes but also ease the burden of frequent imaging on young patients and their families. The ability to effectively predict cancer recurrence can lead to timely interventions and personalized treatment plans, highlighting the importance of integrating technology with medical practices. As research progresses, the threshold for understanding and addressing cancer recurrence in pediatric patients continues to shift, promising a brighter future for brain tumor treatment and management.
The landscape of pediatric oncology is changing dramatically with the emergence of modern predictive technologies, particularly through the use of machine learning models. These advanced tools are capable of providing insights into the potential relapse of childhood cancers, especially those impacting the brain. By utilizing advanced imaging techniques, such as MRI imaging in children, healthcare professionals can analyze longitudinal data to identify at-risk patients more effectively than ever before. This not only streamlines the follow-up process for young patients but also affords them the opportunity to receive tailored therapies based on their unique risk profiles. As innovations in cancer recurrence prediction evolve, the potential for integrating artificial intelligence into clinical practices marks a significant leap forward in pediatric cancer care.
The Potential of AI in Pediatric Cancer Prediction
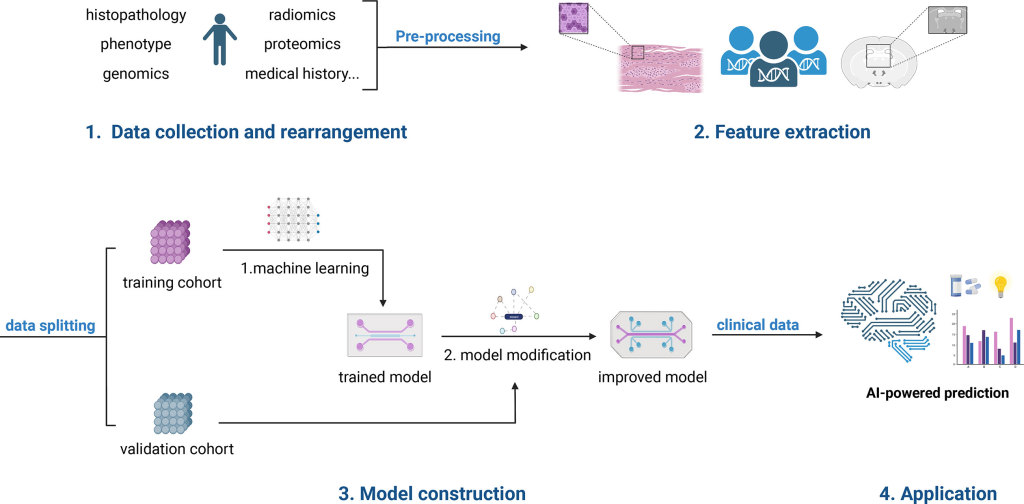
The advancement of artificial intelligence (AI) in medicine has opened new frontiers in the prediction and management of pediatric cancer. In particular, AI prediction pediatric cancer models have shown remarkable potential in enhancing the accuracy of cancer recurrence forecasts among young patients. This shift away from traditional, less reliable methods marks a critical juncture in oncological care, ensuring that clinicians can provide tailored interventions that cater to each child’s unique risk profile.
By leveraging AI tools that analyze extensive datasets—including brain images derived from MRI scans—healthcare professionals can decode subtle patterns that humans might overlook. Such technologies not only promise improved prediction of pediatric gliomas but can also lead to more personalized treatment plans that consider the likelihood of recurrence. This enhances the overall prognosis and quality of care for children battling brain tumors.
Advancements in MRI Imaging for Better Cancer Outcomes
Magnetic resonance imaging (MRI) plays a vital role in the management of pediatric gliomas, as it allows for detailed visualization of brain tumors. However, the traditional approach of using individual scans can lead to inconsistencies in assessing tumor activity. Recent advancements, particularly the integration of AI tools using temporal learning, enable the analysis of multiple scans over time, yielding a more comprehensive picture of tumor behavior and potential recurrence.
Through continuous monitoring and the synthesis of multiple MR images, clinicians can refine their understanding of each patient’s condition, facilitating early interventions when necessary. This progressive methodology emphasizes the critical importance of follow-up imaging in the care of pediatric patients. With AI predicting outcomes more reliably, the stress and burden associated with frequent imaging are likely to diminish, paving the way for a streamlined, less invasive approach to brain tumor management.
Understanding Pediatric Gliomas and Their Treatment
Pediatric gliomas are a type of brain tumor commonly found in children, characterized by their varied histological profiles and potential for recurrence. Many pediatric patients diagnosed with gliomas can achieve favorable outcomes through surgical resection, yet the specter of cancer recurrence looms large, necessitating vigilant follow-up care. Understanding the underlying biology of these tumors is crucial for planning effective treatment protocols, as is the integration of advanced diagnostic tools like AI.
Innovative treatment strategies, such as targeted therapies and adjuvant treatments, are being explored to manage the recurrence of gliomas in pediatric patients. Coupling these strategies with predictive analytics powered by artificial intelligence provides a multidimensional approach to care. The insights gained from AI predictions can assist clinicians in making informed decisions, benefitting from timely interventions that could prevent or mitigate the impacts of recurrence.
The Role of Temporal Learning in Cancer Recurrence Prediction
The introduction of temporal learning in AI models represents a breakthrough in the landscape of pediatric oncology. This approach shifts the focus from isolated image assessments to an analysis of successive MRI scans over time, allowing for a nuanced understanding of tumor dynamics. By recognizing gradual changes rather than relying on static images, the temporal learning model enhances the prediction of cancer recurrence in pediatric glioma patients.
Temporal learning empowers clinicians to gather vital information from various time points post-treatment, facilitating early detection of potential relapses. Researchers have found that this innovative method achieves superior accuracy rates in predicting recurrences compared to traditional single-image analyses. This innovation is pivotal, as it not only addresses the complexities of pediatric gliomas but also elevates the standard of patient care through precise monitoring and intervention.
Impact of AI on Pediatric Oncology Treatments
The incorporation of AI into pediatric oncology is revolutionizing how healthcare providers approach treatment plans for young patients facing brain tumors. With AI prediction pediatric cancer tools, doctors can identify which patients are at a heightened risk of tumor recurrence, leading to more proactive care strategies. This shift can result in personalized therapies that cater to individual needs and significantly improve patient outcomes.
For instance, if AI indicates a high likelihood of recurrence, clinicians may consider implementing adjuvant therapies alongside standard treatments. Conversely, patients identified as low-risk might avoid unnecessary stress and invasive imaging procedures, thereby improving their quality of life. The transformative potential of AI in medicine not only enhances clinical decision-making but also assures families of more effective management of pediatric cancer.
Challenges and Future Directions in AI for Pediatric Cancer
While the promise of AI in predicting pediatric cancer outcomes is exciting, several challenges must be addressed before these tools can be widely implemented in clinical practice. Issues related to data privacy, algorithm bias, and the need for extensive validation across diverse populations are critical hurdles. Additionally, integrating AI tools into existing healthcare workflows poses logistical challenges that need thoughtful consideration.
Future research will focus not only on refining AI models but also on ensuring they complement clinical expertise rather than replace it. As we move forward, collaboration among researchers, clinicians, and technologists will be essential to harness the full potential of AI in pediatric oncology. By overcoming current obstacles, we can ensure that AI becomes a practical asset in the fight against pediatric gliomas and other forms of childhood cancer.
Parental and Family Engagement in Pediatric Cancer Care
The involvement of parents and families in the care of children with pediatric cancer is paramount. As patients undergo treatment for brain tumors such as gliomas, families must often navigate complex medical information and treatment protocols. Enhancing communication between healthcare providers, patients, and families is essential for fostering a supportive environment that prioritizes patient well-being.
AI tools have the potential to bridge gaps in understanding, providing families with insights into their child’s treatment progress and recurrence risk. By simplifying technical information about MRI imaging and AI prediction models, healthcare providers can empower families to make informed decisions regarding care plans. Engaging families effectively creates a more comprehensive care approach, aligning treatment goals with the needs and expectations of patients and their loved ones.
Clinical Trials and AI Research in Pediatric Oncology
The landscape of pediatric oncology is ever-evolving, with ongoing clinical trials exploring the integration of AI in managing pediatric gliomas. These trials aim to assess the effectiveness of AI tools in real-world settings and determine their impact on treatment outcomes and quality of life for young patients. Successful implementations of AI can potentially streamline care protocols and establish new standards in pediatric cancer treatments.
Furthermore, collaboration between hospitals and research institutions is crucial to harness the collective expertise and resources needed for rigorous testing of AI models. By focusing on structured trials that engage diverse pediatric populations, researchers can ensure that AI-driven solutions are both effective and equitable, ultimately paving the way for improved childhood cancer care across the board.
The Future of Pediatric Brain Tumor Treatment and AI Advances
Looking ahead, the future of treatment for pediatric brain tumors is increasingly intertwined with advancements in AI technology. The ability of AI prediction models to analyze data from multiple MRI scans will likely lead to a paradigm shift in how clinicians approach monitoring and treating pediatric gliomas. Such progress not only aims to enhance the accuracy of predictions but also to inform targeted, personalized treatment strategies for children facing cancer.
As AI continues to evolve, it is integral for healthcare systems to adapt accordingly. Continuous investment in research, education, and resources will be vital for maximizing the impact of AI in pediatric oncology. The goal is to not only improve clinical outcomes but also to ensure that pediatric patients with brain tumors receive compassionate, personalized care that prioritizes their overall health and well-being.
Frequently Asked Questions
How does AI prediction improve outcomes for pediatric gliomas?
AI prediction enhances outcomes for pediatric gliomas by accurately predicting cancer recurrence. Using advanced algorithms, AI analyzes multiple MRI scans over time, allowing for early identification of relapse risk, which is crucial for timely treatment interventions.
What role does MRI imaging play in AI prediction for pediatric cancer?
MRI imaging is vital in AI prediction for pediatric cancer as it provides comprehensive data. AI models use this imaging to learn from serial scans, enabling better predictions of pediatric glioma recurrence and improving overall treatment strategies.
What is the significance of cancer recurrence prediction using AI in children?
Cancer recurrence prediction using AI is significant for children with brain tumors because it helps in developing personalized treatment plans, minimizes unnecessary follow-ups, and reduces the anxiety associated with frequent imaging.
Can AI prediction tools help in brain tumor treatment for children?
Yes, AI prediction tools can significantly aid in brain tumor treatment for children by accurately forecasting the risk of tumor recurrence, which allows for better-tailored treatment options and improves management of pediatric gliomas.
What advancements are being made in AI and medicine for predicting pediatric cancer outcomes?
Recent advancements in AI and medicine have led to the development of predictive models that utilize temporal learning strategies. These models analyze longitudinal MRI imaging data from pediatric patients, resulting in higher accuracy in predicting cancer recurrence, especially for pediatric gliomas.
How accurate are AI predictions for pediatric cancer recurrence?
AI predictions for pediatric cancer recurrence, particularly for gliomas, have shown accuracy rates between 75-89%. This is significantly higher than traditional prediction methods based on single MRI scans, which typically have around 50% accuracy.
What is temporal learning in the context of AI prediction for pediatric gliomas?
Temporal learning in AI prediction involves analyzing a series of MRI images collected over time to detect subtle changes that indicate tumor recurrence. This method enhances the model’s ability to predict outcomes more effectively than using individual scans.
Are there plans for clinical trials to validate AI predictions in pediatric cancer?
Yes, researchers are planning clinical trials to validate AI predictions in pediatric cancer. These trials aim to determine if AI-informed predictions can improve patient care by optimizing imaging frequency and treatment approaches for different risk levels.
| Key Point | Details |
|---|---|
| AI tool for predicting relapse | An AI tool accurately predicts the risk of relapse in pediatric cancer patients, outperforming traditional methods. |
| Focus on pediatric gliomas | The study primarily emphasizes improving care for children with gliomas, which are often treatable but have varying recurrence risks. |
| Temporal learning method | The researchers used a temporal learning method to analyze multiple MR scans over time, enhancing predictive accuracy. |
| Study findings | The temporal learning model achieved 75-89% accuracy in predicting recurrence within one year post-treatment, compared to 50% with single image analysis. |
| Future implications | The researchers aim for clinical trials to validate AI predictions for better patient care, potentially reducing imaging for low-risk patients. |
Summary
AI prediction in pediatric cancer is poised to revolutionize how we understand and manage treatment for young patients. By leveraging advanced techniques like temporal learning, researchers are able to offer more precise predictions regarding relapse in pediatric gliomas. This not only alleviates the stress of frequent imaging but also provides opportunities for tailored treatment approaches, paving the way for improved outcomes in young patients fighting cancer.